Diabetic Ketoacidosis Is Preventable With Proper Treatment
Diabetes is 1 of the top 3 common chronic conditions in the United States that leads to death and disability and is the 7th-leading cause
of death.
Cancer, diabetes, and heart disease-account for a large
portion of the $3.3 trillion annual US health care expenditures. In fact, 90%
of these expenditures are due to chronic conditions. About 23 million people in
the United States have diabetes, 7 million have undiagnosed diabetes, and 83
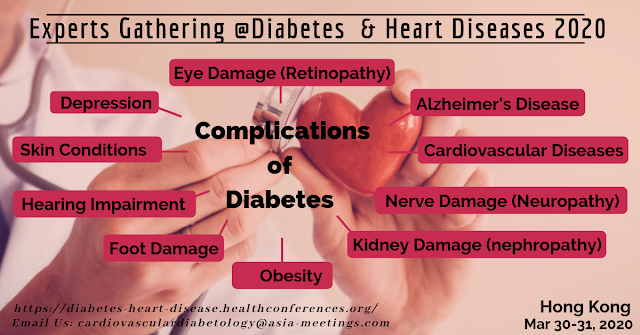
million have prediabetes. Untreated diabetes can become life-threatening, and
the disease is the No. 1 cause of adult blindness, kidney failure, and
lower-limb amputation. Of these life-threatening complications, diabetic
ketoacidosis (DKA) is the leading cause of death in type 1 diabetes (T1D)
and is preventable with proper treatment.
DKA is characterized by hyperglycemia (>250 mg/dL),
increased ketones, and metabolic acidosis. DKA develops when diabetes, usually
T1D is uncontrolled and the body does not have enough insulin to allow glucose
into cells and be used for energy. Once this happens, glucose continues to
accumulate in the blood and the liver starts to breakdown fat into ketones. In
a rare circumstance, it is possible to have DKA with a blood sugar of less
than 200 mg/dL. This is called euglycemic DKA, and it is hypothesized that it
could be caused by chronic liver disease, decreased caloric intake, glycogen
storage disorders, heavy alcohol consumption, pregnancy, recent insulin use, or
recent use of sodium-glucose cotransporter 2 inhibitors.
DKA is a rare, life-threatening condition that can occur
with T1D and occasionally type 2 diabetes. DKA is often the first presenting
symptom of T1D in children and it is also more common in younger people with
T1D, especially those younger than 19. It is estimated that DKA at the initial
presentation is between 13% and 80%, varying greatly by region. For example,
the frequency of DKA at diagnosis is as high as 67% in Romania and 80% in the United Arab Emirates and as low as 13% to 14% in Sweden. Among people who have
T1D, the rate of DKA can be as high as 100% in countries such as Algeria,
Morocco, and Tunisia. Some research has found that patients who experience DKA
at initial presentation may have been experiencing DKA symptoms for more than 2
weeks. The symptoms may go unrecognized not only by caregivers and patients but
by clinicians. Greater awareness of this condition is needed to prevent this
disease from progressing into a life-threatening state.
Although T1D only represents about 5% of diabetes, it is 1
of the most common chronic pediatric conditions, and the number of
hospitalizations in the US from DKA been increasing. Between 2000 and 2009, the
number of hospitalizations from DKA decreased, but between 2009 and 2014 the
rate of hospitalizations increased by 54.9%, and people younger than 45 were 27
times more likely to be hospitalized than those older than 65. Interestingly,
even though the rate of hospitalization has been increasing in the United
States, which could be to the result of a multitude of factors, the in-hospital mortality rate in the United States has been decreasing. Those who survive an
episode of DKA may suffer from persistent short-term memory loss and even a
decrease in their intelligence quotient.
To prevent the potentially devastating consequences of DKA,
it is imperative for clinicians to recognize the signs and symptoms of DKA and
T1D and educate caregivers and patients.
Risks for DKA at the time of diabetes diagnosis include
being younger than 5 years of age, with some research showing that children
younger than 2 years have 3 times the risk of presenting with DKA than children
older than 2 years; delayed diagnosis or misdiagnosis; lacking private health
insurance; lower socioeconomic status; or residing in areas with a low the occurrence of T1D.
Risk factors for DKA in children with established T1D include
being younger than 13 years or female; lack of private health insurance, low
socioeconomic background; poor family relations; poor glycemic control;
psychiatric conditions; and taking higher insulin dosages.
Presentation symptoms include abdominal pain; altered level
of consciousness; the breath that smells like fruit, nail polish, or nail polish
remover; coma; decreased appetite or reflexes; difficulty breathing;
disorientation; hypothermia; ill appearance, as DKA may coincide with another
illness, so watch for chills, cough, fever, or malaise; Kussmaul breathing
and/or tachypnea; lethargy; nausea; polyuria; rapid weight loss; signs of
dehydration, such as decreased skin turgor, dry mucous membranes or skin,
hypotension, and tachycardia; vomiting; weakness; and xerostomia.
Prevention of DKA
Diet: Patients should coordinate with all members of their
care team regarding their diet and treatment plan. The care team should ideally
include a registered dietician (RD) who can help manage this complex chronic
condition. An RD can help improve glycemic control and delay the onset of
diabetes complications. Dyslipidemia, hypertension, and nephropathy are associated
with hyperglycemia and obesity. Uncontrolled diabetes increases the risk of
dental, heart, and kidney disease; foot problems; nerve damage; retinopathy;
and stroke. Hypoglycemic episodes can lead to convulsions, death, seizures, or
unconsciousness.
Early recognition of the signs and symptoms of hyperglycemia
before it evolves into DKA.
Exercise: About 60%
of those with T1D are obese or overweight and have dyslipidemia, 40% have
hypertension and most are physical underactive. Patients should discuss how to
start an exercise routine with their care team to maintain safe blood glucose
levels.
Proper insulin use: Managing T1D is complex and requires careful
titration of insulin dosages, which can vary by comorbidities, development,
illness, periods of growth, physical activity, and various other factors.
Patients should also discuss with their care team how often and when to check
blood sugars.
Sufficient
dietary fiber intake: Fiber can help patients manage diabetes by delaying or
reducing glucose absorption, improving low-density lipoprotein cholesterol and
minimizing post-prandial glycemic spikes.
For more details: https://diabetes-heart-disease.healthconferences.org/
Contact Us: +441234982406 / +441888370010